Childhood obesity is becoming more of a problem in the United States. It affects more than 18% of children, giving it the most prevalent chronic childhood illness. Since 1980, this figure has more than quadrupled. Childhood obesity is a public health concern. Diabetes, hypertension, and other co-morbid illnesses linked with obesity & morbid obesity are now being detected in an increasing number of youngsters.
Obesity in childhood is a major medical problem that affects children and adolescents. It's especially concerning since additional pounds frequently set youngsters on the path to health problems that were formerly thought to be adult issues - diabetes, high blood pressure, and high cholesterol. Obesity in childhood can also contribute to low self-esteem and depression. Obesity is defined as having a body mass index (BMI) higher than that of 95% of children who are the same age & gender. If your BMI is more than 120 points higher than the 95th percentile, you are called very obese.
The environment of today has a significant impact on the habits and views of children and teenagers. A significant component is the proliferation of television advertising encouraging unhealthy meals and eating habits. Furthermore, children are surrounded by environmental forces that diminish the value of physical activity.
Although there are several causes of childhood obesity, some variables have been identified as key contributors to this epidemic. Among the causes are:
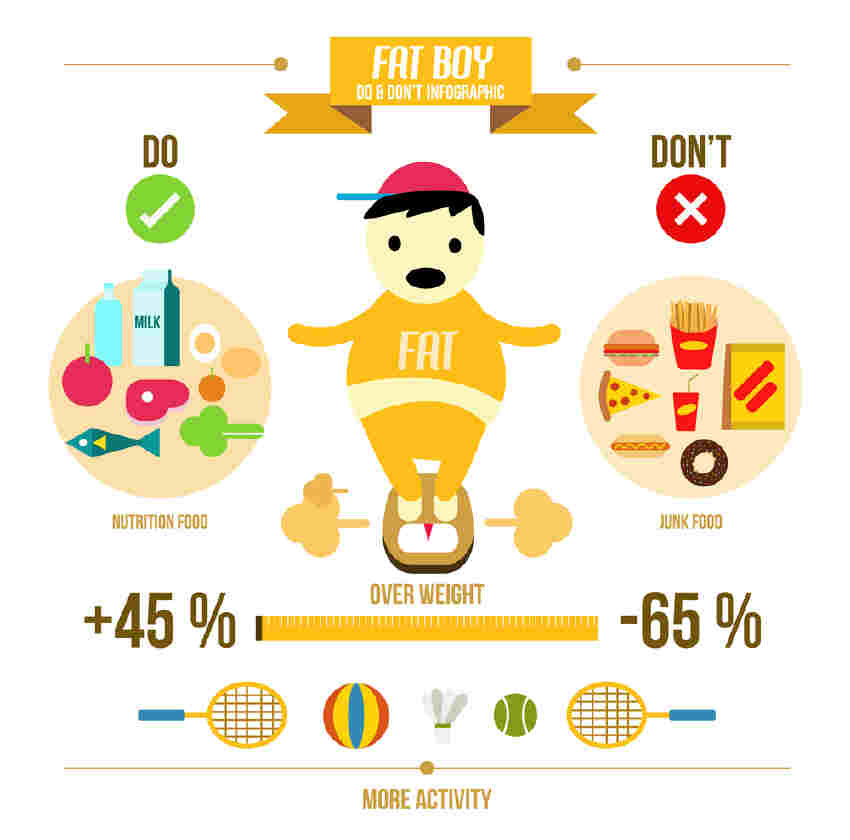
Lack of physical activity: Children who do not exercise regularly are more prone to acquire weight because they do not burn as many calories as those who do. Sedentary activities, such as watching or playing video games, add to the condition as well. TV shows frequently incorporate advertisements for harmful meals.
Heredity and Family: Obesity is genetically determined, according to science. It has been established that children whose parents are obese are more likely to be impacted themselves. According to estimates, genetics accounts for 5 to 25% of the risk of obesity. However, genes alone may not necessarily determine whether a kid is overweight or obese. Parents' learned actions play a significant role. Parents, particularly those whose children are at risk of obesity at a young age, should encourage good eating and lifestyle choices from an early age.
Dietary Patterns: Dietary habits have shifted dramatically during the last few decades. The average number of calories consumed every day has skyrocketed. Furthermore, as calorie consumption has increased, so have the nutrients required for a balanced diet.
Socioeconomic status: Some towns' residents have limited resources and easy access to stores. As a result, individuals may choose nonperishable convenience items such as frozen dinners, crackers, and cookies. People who reside in low-income areas may also lack access to a safe environment to exercise.
Beverages like soda and juice boxes also contribute significantly to the kid obesity pandemic. It is not unusual for a 32-ounce beverage with around 400 calories to be sold to youngsters. Children's soda intake has climbed by 300 percent over the previous 20 years. Scientific research has shown that every ordinary soda taken per day increases the risk of obesity by 60%. Another big issue is the consumption of box drinks, juice, fruit drinks, and sports drinks. These beverages contain a large number of calories, and it is believed that 20% of overweight children are overweight as a result of excessive caloric consumption from beverages.
Treatment of childhood and teenage obesity differs from the treatment of adults. Involving the family in a child's weight control program is an important part of the treatment process. Family, as a support system, is critical in achieving weight control objectives. It is critical to consult with your doctor about treatment options for pediatric obesity. Obesity treatment options for children and teenagers include:
Nutritional treatment: When treating an obese kid or teenager, it is typically advised that they contact a nutritionist who specializes in children's requirements. Nutritionists are the ideal people to assist youngsters to learn good eating habits and ways to incorporate them into their long-term diet.
Physical exercise: Increasing physical exercise is another method of treating childhood obesity. Physical exercise is a crucial long-term component for children since research shows that childhood inactivity is connected to a sedentary adult lifestyle. Increased physical exercise can reduce, or at least halt, the growth of fatty tissues in obese children. The Surgeon General of the United States advises that youngsters engage in at least 60 minutes of physical exercise every day. Individualized programs are accessible and feasible for children and adolescents who are unable to reach minimal standards.
Modification of Behavior: At an early age, lifestyles and habits are formed. Parents and children must be informed and focused on adopting long-term healthy lifestyle choices.
Surgery: While surgery on teenagers has been conducted in extreme circumstances to alleviate obesity, it is only considered for individuals with serious medical issues that can be treated by surgery.

BMI-for-age percentiles are used to determine childhood obesity. BMI-for-age percentiles have been established as the preferred way for assessing children's weight status. This approach determines your child's weight category based on their age and BMI, which is a weight-to-height calculation. However, keep in mind that this approach, like others, should only be used as a tool and that only a physician can adequately identify and diagnose your child's weight condition.
Children's Growth Examination
Your physician may have mentioned your child's weight in terms of percentile. Doctors most usually use weight-for-age percentiles to estimate your child's growth depending on their weight. Weight-for-age percentiles are used to determine your child's weight based only on his or her age. It does not take a child's height into consideration. This is not a tool for determining childhood obesity (or overweight), but rather an indication of growth in comparison to children of the same age.
Risk in Childhood Obesity
Type 2 diabetes is a chronic disease that alters how your child's body processes sugar (glucose). Obesity as well as a sedentary lifestyle both raises the chance of developing type 2 diabetes.
High blood pressure with high cholesterol your child may acquire one or both of these illnesses as a result of a bad diet. These variables can contribute to plaque development in the arteries, causing them to constrict and stiffen, perhaps leading to a stroke or heart attack later in life.
Joint discomfort and extra weight put additional strain on the hips and knees. Childhood obesity can result in hip, knee, and back discomfort, as well as injuries.
Breathing difficulties Children who are overweight are more likely to get asthma. These youngsters are also more prone to develop obstructive sleep apnea, a potentially fatal disease in which a child's breathing stops and begins frequently throughout sleep.
Nonalcoholic fatty liver disease (NAFLD) is a condition in which fatty deposits accumulate in the liver and cause no symptoms. Scarring and liver damage can result from NAFLD.
If you or any of your known is suffering from this disease then click on this link to book an appointment with the best paediatrician: Click here

.webp)